Advanced Specialty Services in Reno, NV
Why race across town to dentists you don’t know? We provide comprehensive, specialized dental care for your entire family in one familiar place.
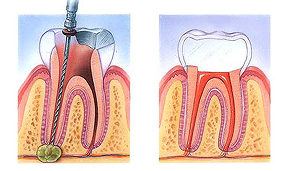
In the past, if you had a tooth with a diseased nerve, you’d probably lose that tooth. Now, with “root canal therapy,” your tooth can be saved. When a tooth is cracked or has a deep cavity, bacteria can enter the pulp tissue and germs can cause an infection inside the tooth. If left untreated, an abscess may form. If the infected tissue is not removed, pain and swelling can result. This can injure your jawbones and be harmful to your overall health.
Root canal therapy involves one to three visits. During treatment, your general dentist or endodontist removes the affected tissue. Next, the interior of the tooth will be cleaned and sealed. Finally, the tooth is filled with a dental composite. If your tooth has extensive decay, your dentist may suggest placing a crown to strengthen and protect the tooth from breaking. As long as you continue to care for your teeth and gums with regular brushing, flossing, and checkups, your restored tooth can last a lifetime.
What is a root canal procedure?
A: Tooth decay can progress down into the pulp. When this happens, the pulp can become infected. Infection of the pulp can be very painful and can also deteriorate into an abscessed tooth when infection and swelling develops in the tissues around or beneath the tooth. When the pulp becomes infected or the tooth becomes abscessed, it is necessary to perform a root canal.
Why do I feel pain?
A: When the pulp becomes infected due to a deep cavity or fracture, bacteria can seep in. When there has been an injury due to trauma, the pulp can die. Damaged or dead pulp causes increased blood flow, pressure, and cellular activity. Pain in the tooth is commonly felt when biting down or chewing, and eating or drinking hot and/or cold foods and beverages.
Why do I need root canal therapy?
A: The tooth will not heal by itself. Without treatment, the infection will spread. The bone around the tooth will begin to degenerate, and the tooth may fall out. Pain usually worsens until one is forced to seek emergency dental attention. The only alternative is extraction of the tooth, which can cause the surrounding teeth to shift, resulting in a bad bite. Though an extraction is cheaper, the space left behind will require an implant or a bridge, which can be more expensive than root canal therapy. If you have the choice, it’s always best to keep your original teeth.
What are the risks and complications of root canal therapy?
A: More than 95 percent of root canal therapies are successful. However, sometimes a case needs to be redone due to diseased canal offshoots that went undetected, or the fracturing of the canal filling. More commonly, a root canal therapy will fail altogether, marked by the return of pain.
What happens after root canal therapy?
A: Once root canal therapy is completed, the endodontist will refer the patient back to our office for the permanent restoration on the tooth. A temporary filling was placed immediately following the root canal therapy and will need to be replaced with a permanent filling or crown and build up. A crown will be necessary on all posterior teeth to properly protect the root canal- treated tooth from fracturing. Front teeth can typically be restored with a filling, however a crown may be necessary in some cases. Your dentist will determine the best choice for your individual needs.
How long will the restored tooth last?
A: Your restored tooth could last a lifetime, if you continue to care for your teeth and gums. However, regular checkups are necessary. As long as the root(s) of a treated tooth are nourished by the tissues around it, your tooth will remain healthy.
How does root canal therapy saved my tooth?
- An opening is made through the crown of the tooth into the pulp chamber.
- The pulp is removed, and the root canals are cleaned, enlarged and shaped.
- Medications may be put in the pulp chamber and root canal(s) to help get rid of germs and prevent infection.
- A temporary filling will be placed in the crown opening to protect the tooth between dental visits. Your dentist may leave the tooth open for a few days to drain. You might also be given medicine to help control infection that may have spread beyond the tooth.
- The temporary filling is removed and the pulp chamber and root canal(s) are cleaned and filled.
- In the final step, a gold or porcelain crown is usually placed over the tooth.
Sleep Apnea Treatment
Snoring and obstructive sleep apnea can lead to serious medical problems.
If you think you may have sleep apnea, please take complete our online questionnaire. If you have been diagnosed with sleep apnea and cannot tolerate the CPAP, our office can help.
Improperly treated obstructive sleep apnea can increase the risk for heart attack, stroke, diabetes and other serious illnesses. Choosing a sleep-disorders dentist who is qualified to work with your physician is essential to your health or the health of a loved one.
Obstructive sleep apnea is a serious medical problem that has been associated with cardiac problems, high blood pressure, stroke, diabetes, ED, gastro-esophageal reflux disease, and numerous other medical problems. Neither snoring nor sleep apnea should be taken lightly, as your health is at stake. Recent research is beginning to explore the complex interrelationships between sleep apnea and these other medical problems. Management by a dentist should always involve interaction with your family physician, cardiologist, pulmonologist and/or endocrinologist.
The dentist you choose to treat your problem with sleep disordered breathing must be properly educated and with adequate experience. Legally, any dentist can treat snoring and/or sleep apnea with an oral appliance, however, that does not mean that every dentist has the necessary experience and training to provide proper therapy. Because no special qualifications are required it is your responsibility to choose your dentist wisely. A qualified sleep-disorders dentist should have:
- Appropriate knowledge of sleep medicine
- Adequate training in oral appliance therapy
- Experience with many different appliance types
- Solid relationships with local sleep labs and sleep physicians
- Current knowledge of emerging trends
- Ability to derive maximum insurance benefits for you
- A team approach with other professionals
- A proven follow-up system to ensure healthy results long-term
- In-depth knowledge of oral appliance research
TMJ Treatment
Advanced Solutions for TMJ
Do you suffer from chronic pain in your jaw and face, experience “popping” sounds when you chew and talk or have symptoms such as headaches or lockjaw? If so, the problem may be TMJ. This condition affects more than 10 million people in the U.S. alone. And it’s more than just painful — over time it can cause serious damage to your jaws and teeth.
TMJ Dysfunction is a popular term to describe a disorder of the jaw joints or the muscles that control the joints. Symptoms masquerade as a multitude of other problems such as sinus headaches, migraines, neck and shoulder stiffness and earaches.
We can accurately pinpoint the source of your pain and provide relief using the very latest in gentle, nonsurgical treatments.
